GMP for Advanced Therapy Medicinal Products (ATMPs) (Part II) and hospital exemption (HE)
- 14 February 2018
- advanced therapy medicinal product, aseptic manufacturing, ATMP, biosafety, clinical trials authorisation, CTA, data integrity, decentralized manufacturing, GMO, GMP, HE, hospital exemption, IMP, investigational medicinal product, MAH, manufacturer, manufacturing, manufacturing platform, marketing authorisation, marketing authorisation holder, operating theatre, process validation, risk assessment, sponsor, unmet medical needs,
On 22 November 2017, the European Commission (EC) has adopted and published Guidelines on Good Manufacturing Practice specific to Advanced Therapy Medicinal Products, one of the initiatives of the Action Plan for ATMPs launched in October 2017 to foster the development of ATMPs. Advanced Therapy Medicinal Products (ATMPs) manufacturers should comply with these Guidelines no later than 22 May 2018.
The new Guidelines, developed after extensive consultation with stakeholders, EMA and competent national authorities, adapt the GMP requirements to the specific characteristics of ATMPs.
We have already informed on our website about a consultation document on GMP for ATMPs published by European Commission (EC) for public consultation in June 2016 as well as about a concern expressed by PIC/S Committee related to the European Commission’s proposal of stand-alone Advanced Therapy Medicinal Products (ATMPs) GMP Guidelines.
ATPMs are medical products for human use based on genes or cells that offer potentially ground-breaking opportunities for the treatment of injury and disease, particularly in cases of severe, untreatable or chronic diseases which do not respond adequately to conventional treatments.
In the EU, these products are governed by Regulation (EC) No 1394/2007 on advanced therapy medicinal products (“ATMP Regulation”). The cornerstone of the Regulation is that a marketing authorisation must be obtained prior to the marketing of ATMPs. The evaluation of these products is led by a specialised committee within the European Medicines Agency (the Committee for Advanced Therapies – “CAT”) and the authorisation is granted by the European Commission. Since 2009, EMA has been reviewed 15 applications for marketing authorisation resulting in 8 approved ATMPs (3 had been withdrawn) – data reported in January 2017.
The ATMP Regulation (under Article 28(2)) also empowers Member States to permit the use of advanced therapies that have not been authorised by the Commission under certain conditions (so-called “hospital exemption”). The hospital exemption applies only to custom-made ATMPs used in a hospital setting for a specific patient. Such products are produced under the responsibility of a physician and are only to be used within the Member State where it is produced (unlike centrally authorised ATMPs). In addition, a competent authority must authorise hospital exemption for ATMPs and they must comply with the same national requirements concerning quality, traceability and pharmacovigilance that apply to authorised medicinal products.

The hospital exemption is an important tool to facilitate access of patients to new treatments for unmet medical needs. However, the use of hospital exemption in lieu of the authorisation route to the market deprives large groups of patients across Europe of the benefits of therapy. Similarly, divergent implementation of Article 28(2) in different Member States could have a negative impact on patient access to treatments as well as ATMP development. It should be noted, however, that hospital exemption facilitates research and development in advanced therapies by non-profit organisations (such as academia and hospitals) and it can be a valuable tool to obtain information prior to seeking a marketing authorisation. Clinical trials however, must remain the preferred route for generating clinical data.
Update [30/04/2020]
As was mentioned above, hospital exemption for advanced therapy medicinal products (ATMPs) is part of the EU pharmaceutical framework, but its application is a national competence.
Taking into account the divergent practices across the EU related to the application of Article 28(2) of the ATMP Regulation, discussions among national experts on the application of the hospital exemption are still ongoing.
Discussion topics include:
- elements to define “non-routine” basis of production/use of an ATMP in a hospital;
- decentralised manufacturing;
- boundaries between hospital exemption and Article 5 of Directive 2001/83/EC;
- hospital exemption and clinical trials framework;
- safety monitoring and efficacy monitoring;
- information to patients/advertising and promotion.
The key aim of exchanging views on the application of the hospital exemption is development of a good practice that Members States may decide (or not) to follow when they apply Article 3(7) of Directive 2001/83/EC.
The manufacturing of ATMPs poses unique challenges (e.g. limited availability and intrinsic variability of the starting materials, short shelf-life, very small batch sizes) and the application of GMP has been consistently identified as a problem for ATMP developers. The adaptations introduced in the GMP framework for ATMPs continue ensuring a high level of quality for ATMPs and a high level of patient protection. In addition, the Guidelines are expected to make a significant contribution to the development of these products and will provide increasing opportunities for patients to be enrolled in clinical trials with ATMPs in the EU.
Comparing to the consultation document, generally, final version of Guidelines includes some additional sections while others are changed or stated more precisely. The key differences are presented below.

Chapter 1. Introduction addresses information on the legal basis related to ATMPs. First section of the Guidelines explains that compliance with good manufacturing practice (“GMP”) is mandatory for all medicinal products that have been granted a marketing authorisation. Likewise, the manufacture of investigational medicinal products must be in accordance with GMP. Advanced therapy medicinal products that are administered to patients under Article 3(7) of Directive 2001/83/EC (so-called “hospital exemption”) must be manufactured under equivalent quality standards to the manufacturing of advanced therapy medicinal products with a marketing authorisation.
Additionally, in five sections, a role of marketing authorisation holder/ sponsor is described, particularly regarding necessity of cooperation between the manufacturer and the marketing authorisation holder/ sponsor concerning the manufacturer’s ability to comply with GMP; responsibility of the sponsor/ marketing authorisation holder to ensure that the specifications/ instructions submitted to the manufacturer are in accordance with the terms of the clinical trial authorisation/ marketing authorisation as well as the manufacturer’s responsibility for compliance with the specifications and instructions provided by the sponsor/ marketing authorisation holder; or the obligations of the marketing authorization holder/ sponsor and the manufacturer and vis-à-vis each other which should be defined in writing..
In addition, Pharmaceutical Quality System is described in more detail. Comparing to the consultation document, there are some more requirements, as e.g.:
- results of parameters identified as a quality attribute or as critical should be trended and checked to make sure that they are consistent with each other;
- as part of the pharmaceutical quality system, the manufacturer should conduct self-inspections;
- quality reviews for authorised ATMPs should be conducted annually and the results of the review evaluated and assessed whether corrective and/or preventive actions are required by the manufacturer and -when it is a different legal entity- the marketing authorisation holder.
Chapter 2. Risk-based approach, under p. 2.3.4. Additional considerations relevant for investigational ATMPs addresses in more detail exceptional possibility to manufacture the product- investigational ATMPs in very early phase/proof of concept trials- in an open system in a critical clean area of grade A with a background clean area of grade C; manufacturing of such products is possible if the following (cumulative) conditions are met:
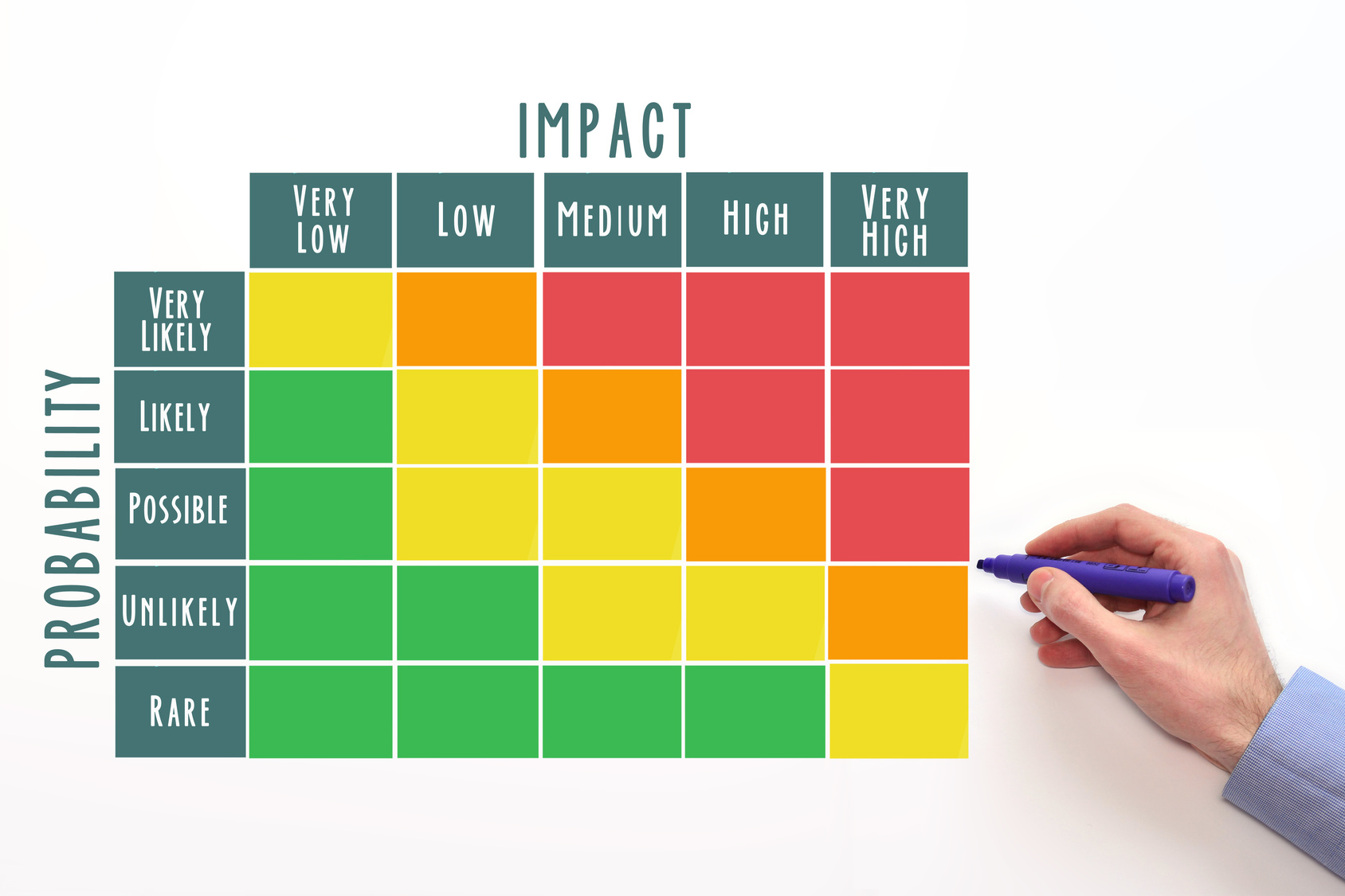
- A risk-assessment has been performed and demonstrated that the implemented control measures are adequate to ensure manufacture of the product of appropriate quality. In addition, the control strategy should be described in the investigational medicinal product dossier.
- The product is intended to treat a life threatening condition where no therapeutic alternatives exist.
- The relevant competent authorities agree (agreement of both the assessors of the clinical trial and the inspectors of the site).
This approach raises concerns of National Competent Authorities (NCAs). National Competent Authorities retain the ability to refuse A/C clean air requirements for FIM investigational ATMPs.
It should be noted, however, that investigational ATMPs should be manufactured in a facility with air quality requirements in accordance with the requirements set out in Sections 4.3.2. and 9.5. of the Guidelines.
Comparing to the consultation document, there are some additional requirements described in p. 3.4. Key personnel, as e.g.:
- in case of ATMPs containing or consisting of GMOs, the person responsible for biosafety should be appointed by senior management;
- the person responsible for production, the person responsible for quality control, and- where applicable- the person responsible for quality assurance, share some responsibilities regarding the design and implementation of the pharmaceutical quality system (e.g. training, process validation, quality investigations).

Under p. 6.1. General principles (Chapter 6. Documentation) more details are given with reference to placing physical and/or logical controls to limit access to computerised system to authorised persons to ensure data integrity. Suitable methods of preventing unauthorised entry to the system may include e.g. the use of keys, pass cards, personal codes with passwords, biometrics, or restricted access to computer equipment and data storage areas. The extent of security controls depends on the criticality of the computerised system.
Processing of starting materials (Chapter 7. Starting and raw materials) – Section 7.35. states: In exceptional cases, it may be acceptable that the manufacture of an ATMP starts from already available cells or tissues where some initial processing/ manufacturing steps have been performed outside of the GMP environment, provided it is impossible to replace such material with GMP-compliant material.
There are some new sections under p. 9.5. Aseptic manufacturing (Chapter 9. Production). One of these new sections relates to manufacturing of the ATMP in the operating theatre. In exceptional circumstances and provided that it is duly justified, closed systems may be placed in a controlled but non-classified environment. The conditions of the operating theatre where the manufacturing activity takes place should be adequate and sufficient to ensure the quality and safety of the product. It is stressed that this is only acceptable in exceptional cases and that the product should not be exposed at any moment to the environment. It should be also demonstrated that the expected clinical benefit for the patient outweighs the risks linked to the absence of a classified background.
There is another important section concerning production in an open system. Generally, when the product is exposed to the environment (e.g. working under laminar air flow), a critical clean area of grade A with a background clean area of grade B is required for aseptic preparation and filling. However, the use of technologies such as e.g. processing inside sterile disposable kits, incubation in closed flasks, bags or fermenters in a grade C environment may be acceptable if adequate control measures are implemented to avoid the risk of cross-contamination (e.g. appropriate control of materials, personnel flows and cleanness). Particular attention should be paid if the materials are subsequently moved to a clean area of higher grade. It should be noted, however, that if the closed flasks, bags, fermenters allow for a full isolation of the product from the environment, these would be considered as closed systems and the relevant principles of closed systems would then apply.



Validation Strategy for closely related products is described in Section 10.45. (Chapter 10. Qualification and validation). Where the same manufacturing platform is used for a number of closely related products (e.g. genetically modified cells where viral vectors are manufactured according to the same manufacturing process), the extent of validation work for each new product should be based on a justified and documented risk assessment of the process. This should take into account the extent of process knowledge, including existing relevant process validation work, for each significant step in the process. Thus, in so far as the other manufacturing steps remain the same, it may be possible to limit the validation to only the steps that are new to the process.
Comparing to the consultation document, there are three additional sections under p. 10.5. Validation of transport conditions. Transport conditions may have a crucial impact on the quality of ATMPs and should be defined in writing. Their adequacy should be demonstrated, however, compliance with them is outside the scope of GMP.
Similarly, new Guidelines address the novel scenario so-called decentralised manufacturing and describe (in nine sections) a batch release process in this particular case (p. 11.3.3. Batch release process in cases of decentralised manufacturing, Chapter 11. Qualified person and batch release). There may be cases where manufacturing of the ATMP needs to take place in sites close to the patient (e.g. ATMPs with short shelf-life, clinical advantage of using fresh cells as opposed to freezing the starting materials/finished product, etc.). In such cases, manufacturing of the ATMPs may need to be decentralised to multiple sites so as to reach to patients across the EU (“decentralised manufacturing”). This scenario may occur both in the context of authorised ATMPs as well as in the context of investigational ATMPs. The batch certification and release process becomes then particularly important as manufacturing in multiple sites increases the risk of variability for the product. In particular, through the batch certification and release process it must be ensured that each batch released at any of the sites has been manufactured and checked in accordance with the requirements of the marketing authorisation/clinical trial authorisation and other relevant regulatory requirements including compliance with GMP.
Reflection on the concept of comparability as it applies to ATMPs is of particular relevance when upscaling manufacturing and with novel manufacturing models (decentralised/ distributed manufacturing).
NEW! Update [18/05/2020]
More information on the comparability exercise for ATMPs you can find here.
Final version of the Guidelines includes also Glossary (at the end of the document).
Source: EC, PC and EMA